Introduction

This Straight, No Chaser looks at mental health as an equivalent of an upcoming pandemic.
The general American population (and perhaps the world in differing amounts) is about to get a up close look at what is known as social determinants of health. With another 5.2 million Americans filing for unemployment (raising the number to over 22 million over the last four weeks), we are reaching a critical mass of economic hardship. As a result, someone (everyone) needs to prepare for the mental health ramifications of this.
Mental Health Challenges

Here are some predictable scenarios, each with mental health consequences:
• Depressions (and even suicide rates) will explode.
• Individuals prone to post-traumatic stress will have flare ups. Also, others will develop an equivalent of it.
• Americans will be forced to choose between food and medicine. Unfortunately, others won’t have either as an option and will become ill (and die) as a result.
• We will become angry. Anger will be expressed; in some cases rightfully so, and it will be displaced inappropriately. Predictably, we have already begun to see demonstrations.
• In some instances, there will be violence. This will range from domestic violence to outward expressions. Sadly, everyone’s fuse is shortening.
How Will You Cope?
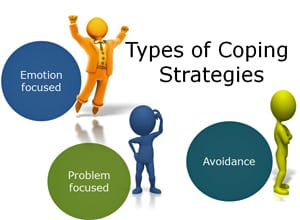
There’s so much more, but you should get the point. The question, of course, is how will you cope with the upcoming pandemic of mental health issues? Do you have the means, inclination and access to get help? Let’s start with self-help measures you can take. From there, just being mindful that these issues will be arising may convince you to get help when you need it. Also take the time to look after those you care for. Actually engage people in conversations about their mental health. For years, I’ve told patients that when I asked them how they were doing, it wasn’t a pleasantry but an actual inquiry. Care enough to do the same. We’re all in this together. When things “return to normal,” maybe show a little empathy for those for whom this has always been their normal.
Straight, No Chaser Posts on Mental Health
Developing a Stress Management Plan
Post-Traumatic Stress Syndrome in Communities
Depression: How to Avoid it and When to Get Help
How to Escape a Domestic Violence Situation
Need Masks?
The CDC now recommends everyone wear masks. Courtesy of SI Medical Supply, you have an option to provide 3-layer facial masks for your family and loved ones. You can now obtain a pack of 15 for $35, including shipping and handling. These are the recommended masks. Importantly, getting this product does not deplete the supply needed by first responders and medical personnel. Orders are now being filled (without shipping delays!) at www.jeffreysterlingmd.com or 844-724-7754. Get yours now. Supplies are limited.

Follow us!
Feel free to #asksterlingmd any questions you may have on this topic. Take the #72HoursChallenge, and join the community. As a thank you, we’re offering you a complimentary 30-day membership at www.72hourslife.com. Just use the code #NoChaser, and yes, it’s ok if you share!
Order your copy of Dr. Sterling’s books There are 72 Hours in a Day: Using Efficiency to Better Enjoy Every Part of Your Life and The 72 Hours in a Day Workbook: The Journey to The 72 Hours Life in 72 Days at Amazon or at www.jeffreysterlingbooks.com. Receive introductory pricing with orders!
Thanks for liking and following Straight, No Chaser! This public service provides a sample what you can get from http://www.docadviceline.com. Please share our page with your friends on WordPress! Like us on Facebook @ SterlingMedicalAdvice.com! Follow us on Twitter at @asksterlingmd.
Copyright © 2020 · Sterling Initiatives, LLC · Powered by WordPress
















 Risks for Suicide at College
Risks for Suicide at College