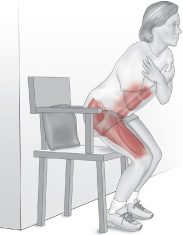
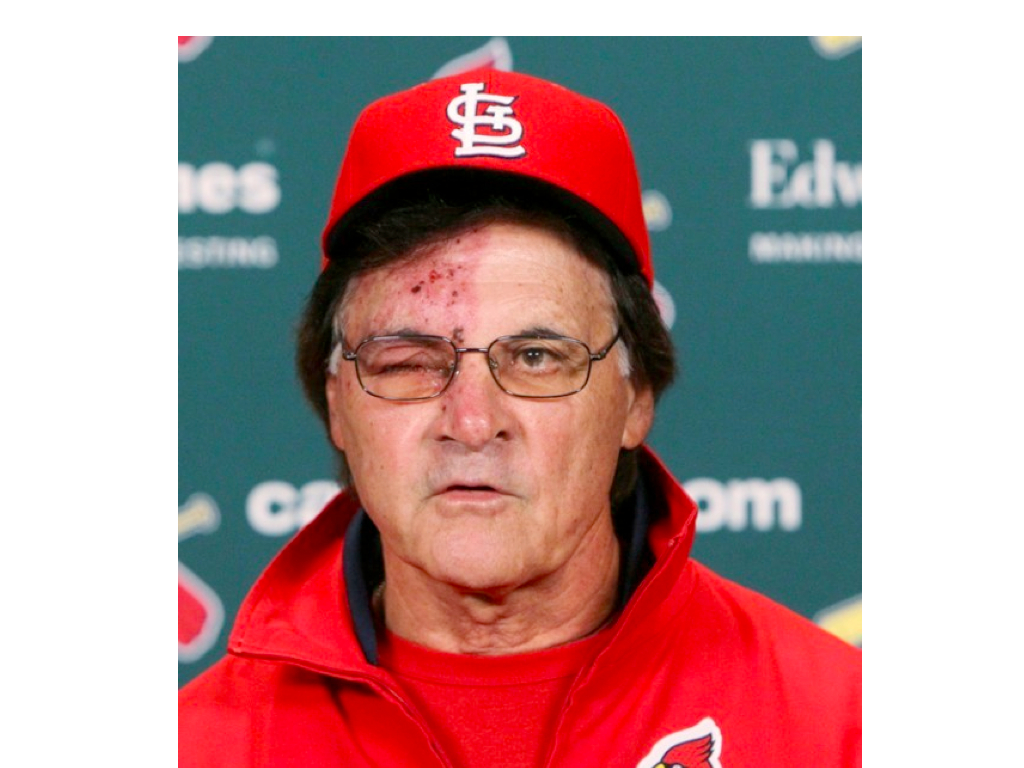
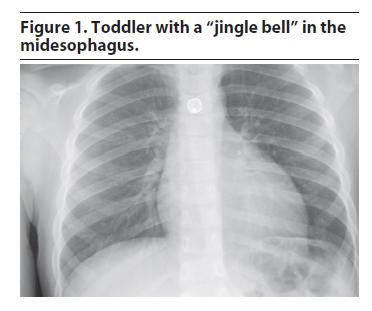
It’s another interesting night in the ER. My nurses are hounding me because there’s a patient with a rash, and they don’t know what it is. They’re so good that they rarely get stumped, and they get excited when they are. The patient had a pretty impressive cluster of little blisters called vesicles (see the picture above) under one eye with significant reddening of the skin under the cluster. Unknown to them, their problem with this patient is she’s African-American. Many healthcare professionals have difficulty identifying common rashes in dark-skinned individuals.
I wonder if any of you haven’t had chickenpox. That’s a question that never would have been asked a few decades ago. Chickenpox is caused by the Varicella Zoster virus, which is one of the Herpes viruses (No not that one; we’ll discuss that next week.). Repeat infections or reactivation of the virus that went dormant inside of you causes shingles. When I was younger, no one ever got shingles because no one got chickenpox twice. Chickenpox was something you got as a child, and when you contracted it, everyone in the neighborhood would bring the kids by so everyone could get it and be done with it. The first case of shingles I actually remember seeing was during residency in a HIV+ patient who actually died from it (Herpes Zoster pneumonia; I was told it happened to the elderly or patients with lowered immunity).
Then an odd thing happened. A chickenpox vaccine came out. Chickenpox started being seen in older individuals, because all the kids were immunized, and the loss of the ‘herd immunity’ phenomenon allowed some individuals to sneak by without getting chickenpox as a child, only to develop it at an older age. Then shingles started being seen more often.
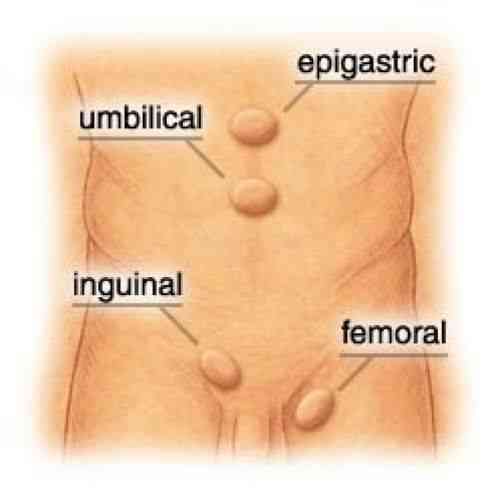
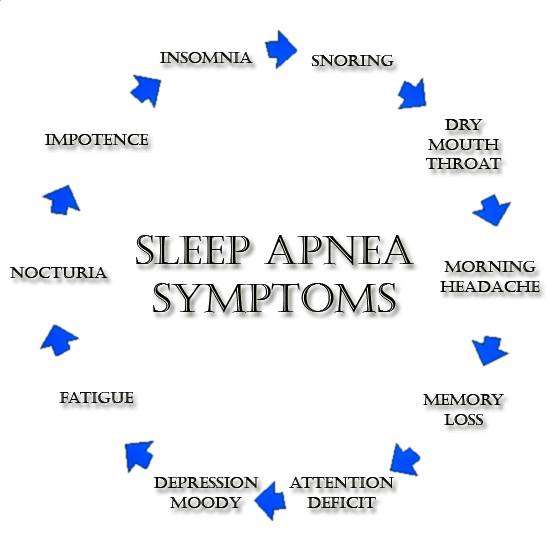
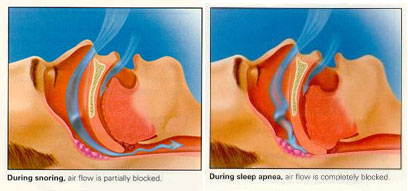
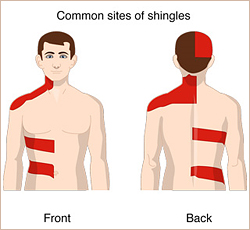
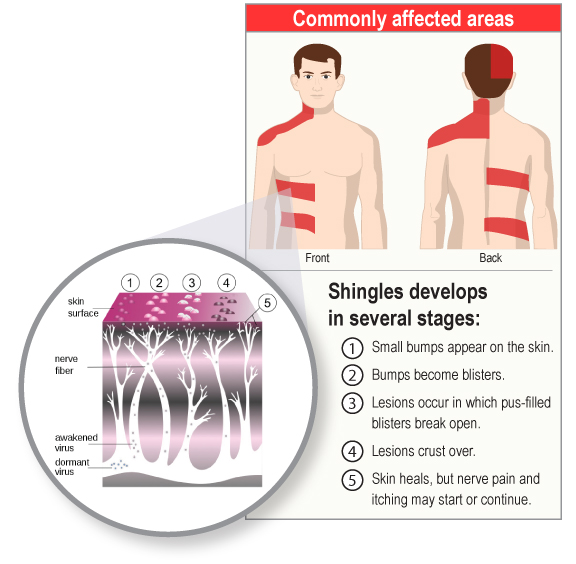
The shingles rash is classically a group of lesions stretched around a single dermatome (an area of skin corresponding to the distribution a specific nerve root), usually in the abdomen or back, but seen with some frequency on the face and involving the nose and around the eyes. Infection begins with general nonspecific symptoms like headache, light sensitivity, pain, itching and burning in the area a few days before the rash appears. The pain should be emphasized, as it can last for a year after the rash (which typically lasts for 2-4 weeks). Amazingly 30 out of 100 Americans will now develop this illness at some point in their lives.
Anyone who has had chickenpox may get shingles. However, you can now get a shingles vaccine, which serves two purposes: it may prevent shingles, but if it doesn’t it can make the episode less painful. If you’re 50, you can get vaccinated, and it can cut the risk of contracting shingles in half. Please discuss this with your physician. If you’re eligible, you’ll thank me; if you don’t get vaccinated and contract shingles, you’ll wish you had.
Quick Tips:
- If you have never had chickenpox and have never gotten the chickenpox vaccine, avoid contact with people who have shingles or chickenpox. Fluid from blisters in both conditions is contagious and can cause chickenpox in these groups.
- If you have shingles, avoid close contact with people until after the rash blisters heal.
- Certain people are at heightened risk from chickenpox and shingles, including anyone pregnant, elderly, ill or with a diminished immune system.
I welcome your questions, comments or stories. For the sports fans out there, this pictorial trivia question shouldn’t be hard to answer. Who’s this famous manager pictured here with shingles?
In the meantime, if you’d like to read Behind the Curtain ahead of its national launch, we are now shipping orders made exclusively on www.jeffreysterlingbooks.com!
Thanks for liking and following Straight, No Chaser! This public service provides a sample of what http://www.SterlingMedicalAdvice.com (SMA) and 844-SMA-TALK offers. Please share our page with your friends on WordPress, like us on Facebook @ SterlingMedicalAdvice.com and follow us on Twitter at @asksterlingmd. Preorder your copy of Dr. Sterling’s new book Behind The Curtain: A Peek at Life from within the ER at jeffreysterlingbooks.com.





























![exercize cat[5]](https://jeffreysterlingmd.com/wp-content/uploads/2014/05/exercize-cat5.jpg?w=300)