There are interesting commonalities of certain drugs like alcohol and cigarettes. One is users that really enjoy them are able to do so for a long time while being oblivious to the growing danger those activities pose. Another commonality is even more so than mentally, when things go wrong physiologically, they really go very wrong.
Possible Complications
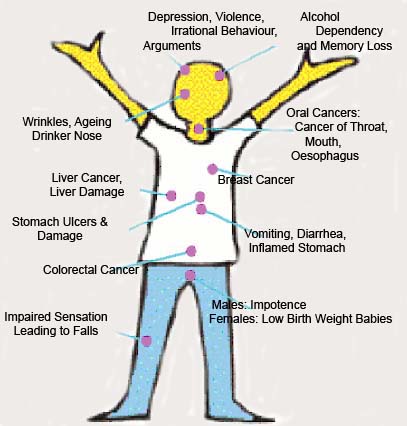
Alcoholism and alcohol abuse pose threats to many aspects of your health, including the following.
- Birth defects (fetal alcohol syndrome)
- Bleeding throughout your digestive tract, including the esophagus (up to and including rupture), gastritis (inflammation of the stomach) and ulcer disease.
- Brain cell damage
- Brain disorder called Wernicke-Korsakoff syndrome (includes dementia, mental status changes)
- Cancer of the esophagus, liver, colon, and other areas
- Changes in the menstrual cycle (period)
- Delirium tremens (DT’s)
- Dementia and memory loss
- Depression and suicide
- Erectile dysfunction
- Heart damage
- High blood pressure
- Increased risks for behavioral disorders including depression and suicide
- Increased risks for sexually transmitted infections (STIs)
- Increased risks for trauma, including motor vehicle collisions, violence and head injuries with intracranial bleeding
- Inflammation of the pancreas (pancreatitis)
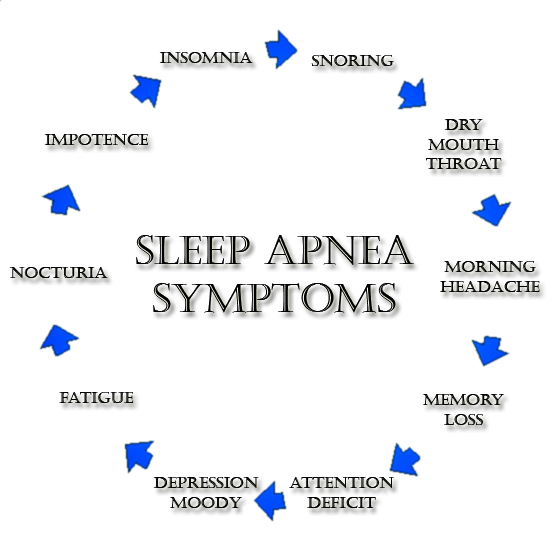
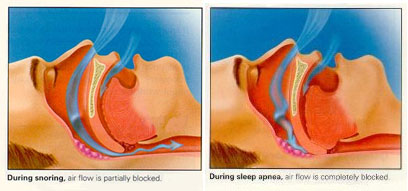
- Insomnia
- Liver disease, including alcoholic hepatitis, cirrhosis and cancer
- Nerve damage
- Nutritional deficiencies
Treatment
Medical goals and patient goals are often different and seem to depend on the extent of perceptible injury that has occurred at the time of the decision to quit drinking. Often, patients will want to reduce drinking instead of stopping completely. Continued drinking in moderation is only as viable an option as the patient’s level of alcohol-related level of disease and the patient’s ability to stay limited in consumption and focused toward that goal.
Ideally, abstinence (the complete stopping of alcohol intake) is the goal, and it needs to be the goal if and when the desire to stop drinking is coupled with the presence of significant alcohol-related disease.
As everyone knows, the management of alcoholism requires multiple simultaneous approaches, including family and social networks. It is often the family network that helps the alcoholic come to the understanding that alcohol intake has disrupted his or her ability to function normally. It is a most unfortunate occurrence when this has not occurred prior to the development of significant medical disease. Individuals with alcohol problems are more likely to take the steps necessary to successfully withdraw from alcohol use.
Regarding the medical aspects of alcohol cessation, withdrawal is a very important consideration and is best done in a controlled manner. Components of effective withdrawal address the various medical and mental health considerations reviewed earlier and medical avoidance treatment.
Medical avoidance treatment includes medicine that prevent relapse via various methods, and they include the following:
- Antabuse (generic name: disulfiram) is a well known and commonly used medicine that works by producing very unpleasant side effects with virtually any alcohol intake within two weeks of taking the medicine.
- Naltrexone (brand name: Vivitrol) is an injectable medicine that works to decrease alcohol cravings.
- Acamprosate is a drug that has been shown to lower relapse rates in those who are dependent on alcohol.
This is part of an ongoing series on alcohol use and abuse.
- Click here to review the symptoms suggestive of alcoholism.
- Additional posts will review a severe form of alcohol withdrawal, delirium tremens (the DTs) and non-medical aspects of treatment.
Feel free to contact your SMA expert consultant if you have any questions on this topic.
Thanks for liking and following Straight, No Chaser! This public service provides a sample of what http://www.SterlingMedicalAdvice.com (SMA) offers. Please share our page with your friends on WordPress. We are also on Facebook at SterlingMedicalAdvice.com and Twitter at @asksterlingmd.