Introduction
It’s endometriosis awareness month, which I’m sure many of you know all too well.
Guys, it’s not condescending to note that it’s really tough to be a woman. There are so many different medical conditions women have to deal with that men don’t. Many of these just don’t even make sense (well, they make medical sense, but not common sense…).
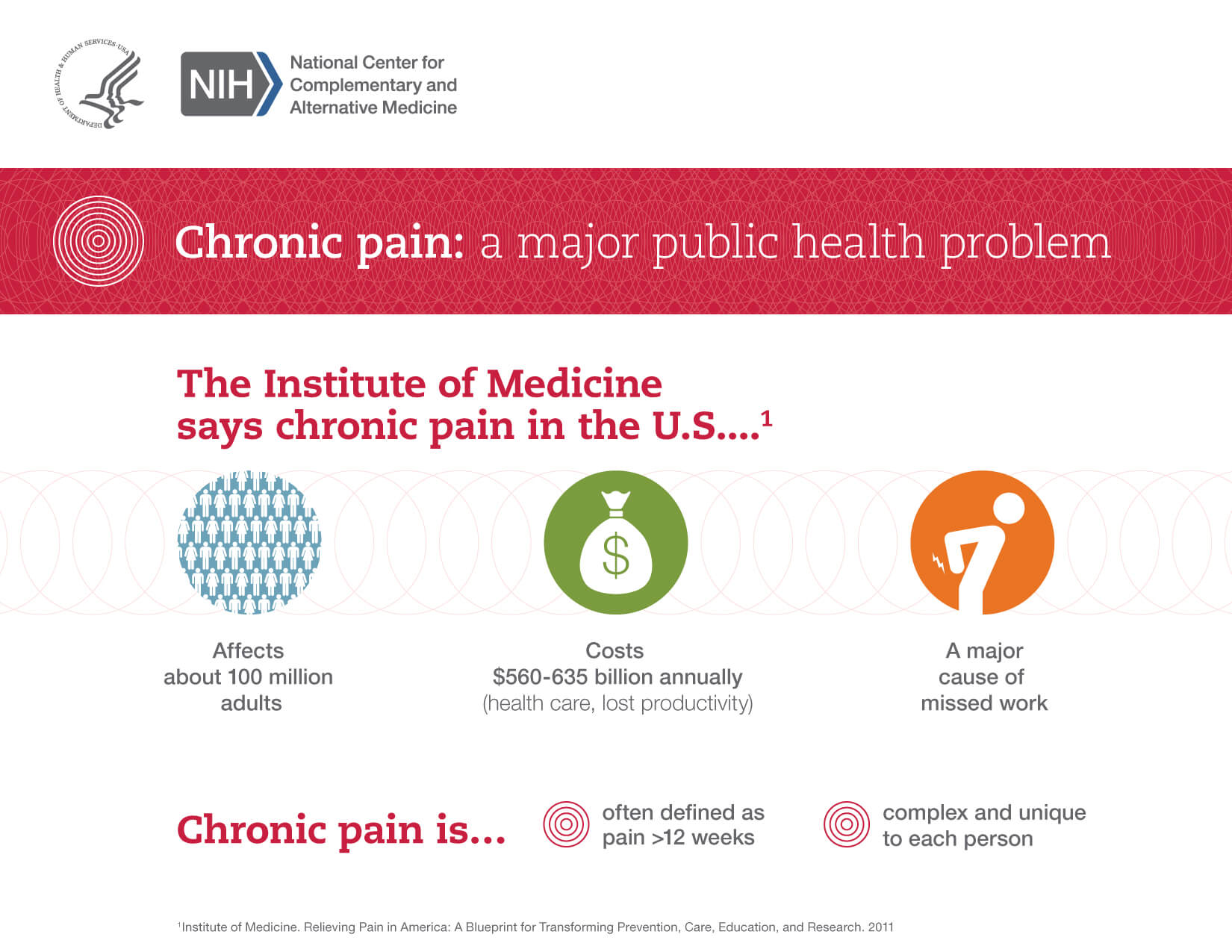
Take the example of endometriosis. Millions of women suffer from this condition, in which cells that are supposed to live and grow in the lining of the womb (uterus), migrate, implant and grow in other parts of the body. What does that mean to the woman? For starters, it means menstrual-type activity that normally occurs in the womb can occur elsewhere. That just seems cruel. In any event, here’s your what, how, why and what to do for endometriosis.
How?
If you understand that every month a woman’s menstrual period represents the shedding of cells from the inner lining of the womb lining, then you’re most of the way to understanding endometriosis. Endometriosis is the result of these shedded cells migrating, implanting and growing outside of the uterus.
Where?
Tissue that migrates from the womb (endometrial lining) most commonly implants onto the ovaries, bladder, intestines, rectum and pelvic lining, although other locations are possible.
Who gets endometriosis?

You’re more likely to develop endometriosis if someone in your family (e.g., mother or sister) has it, if you started your periods at a young age, if you’ve never had children, if your periods are irregular (i.e., frequent or last more than seven days at a time) of if you have a closed hymen (vaginal opening).
What happens next?

One oddity of these endometrial implants is they tend to stay affixed to their new areas in a way that didn’t occur in the womb. Because this is the tissue that is involved in menstruation, they can grow and bleed in conjunction with your menstrual cycle.
What are the symptoms?
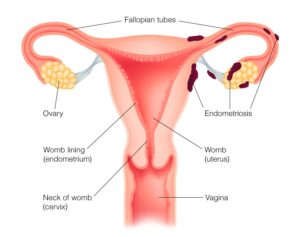
Any, all or none of the following may occur. Actually, endometriosis may exist without symptoms. However, it’s most typically defined by pain.
- Pain during or following sexual intercourse
- Pain with bowel movements
- Painful periods
- Pelvic/low back pain at any time during the menstrual cycle
- Premenstrual and menstrual pain and/or cramping in the lower abdomen
- Intestines obstruction (blockage) or other abnormal functioning (rarely)
How is this figured out?
Your job is to recognize the symptoms and seek assistance. Tests may include a vaginal ultrasound and direct visualization of your pelvis via a procedure called laparoscopy, which also allows for treatment.
How is endometriosis treated?
There’s a wide range of treatment, which depends on your level of health, the presence/significance of symptoms and your desire to have children in the future.
Options range from symptomatic treatment with exercise, relaxation techniques and pain medication to hormonal medications and surgery to remove areas of the endometriosis. The options are assessed and used based on the particulars of each patient.
Endometriosis needs estrogen to grow. Therefore, those with it are advised to keep their estrogen levels low. You can do this by avoiding large consumption of alcohol and caffeinated beverages such as coffee, green tea and soda. Patients with endometriosis should workout 3-4 times a week, as regular exercise keeps estrogen levels low.
What’s the end result?
The treatments mentioned are often effective in improving symptoms but not in providing a cure. A cure is most likely to occur by removal of the womb (uterus), fallopian tubes, and both ovaries (a hysterectomy/oophorectomy).
Complications of endometriosis can include infertility, but this is not universal. More commonly, pain interferes with the activities of daily living. Other complications include formation of large cysts in the pelvis (called endometriomas). Sometimes, post-menopausal cancer presents in the affected areas.
You should get evaluated for endometriosis if a family member has endometriosis or has particularly problematic menstrual periods or if you are having difficulties becoming pregnant (especially after trying for one year).
Follow us!
Ask your SMA expert consultant any questions you may have on this topic. Also, take the #72HoursChallenge, and join the community. Additionally, as a thank you, we’re offering you a complimentary 30-day membership at www.72hourslife.com. Just use the code #NoChaser, and yes, it’s ok if you share!
Order your copy of Dr. Sterling’s books There are 72 Hours in a Day: Using Efficiency to Better Enjoy Every Part of Your Life and The 72 Hours in a Day Workbook: The Journey to The 72 Hours Life in 72 Days at Amazon or at www.jeffreysterlingbooks.com. Another free benefit to our readers is introductory pricing with multiple orders and bundles!
Thanks for liking and following Straight, No Chaser! This public service provides a sample of http://www.SterlingMedicalAdvice.com (SMA) and 844-SMA-TALK. Likewise, please share our page with your friends on WordPress! Also like us on Facebook @ SterlingMedicalAdvice.com! Follow us on Twitter at @asksterlingmd.
Copyright ©2013- 2019 · Sterling Initiatives, LLC · Powered by WordPress