Here’s a quote that I enjoy:
“History favorably remembers those that do things first and those that do things exceedingly well.”
–Anonymous
On this next to last day of Black History month, allow me to use our little corner of the world to recognize and pay tribute to a few of the many African-Americans whose work has impacted the lives of millions around the globe. Even if you are not familiar with these individuals or their work, learning about their existence and pioneering endeavors may prove meaningful.
Dr. James McCune Smith (1813-1865), the first Black to hold a medical degree

James McCune Smith (1813 – 1865) was the first African-American to hold a medical degree, having graduated at the top in his class at the University of Glasgow, Scotland. He was also the first African-American to own and operate a pharmacy in the United States. He has been most well-known for his leadership as an abolitionist, and, along with Frederick Douglass, he helped start the National Council of Colored People (1853), the first permanent national organization for Blacks. Douglass said that Smith was “the single most important influence on his life.”
James Derham (1762-1802?), the first recognized Black physician in the U.S.

James Derham, the first recognized Black physician in the United States, was born a slave in Philadelphia. Owned by a number of physicians, Derham ended up in New Orleans with a Scottish physician who hired him in 1783 to perform medical services. When he turned 21, he bought his freedom, went to New Orleans and established his own medical practice. In 1788, he was invited to Philadelphia to meet Dr. Benjamin Rush, one of the signers of the Declaration of Independence. Rush was so impressed with Derham’s success in treating diphtheria patients that he read Durham’s paper on the subject before the College of Physicians of Philadelphia.
In 1789, Durham returned to New Orleans, establishing his legend; he saved more yellow fever victims than any other physician in colonial Philadelphia. During an epidemic that killed thousands, he lost only 11 of 64 patients. He moved back to New Orleans and was lauded by prominent local doctors. Despite his demonstrated expertise and his flourishing practice, his practice was restricted in 1801 by new city regulations because he did not have a formal medical degree and was unable to get formal training. He disappeared after 1802, and his fate was unknown.
Dr. David Jones Peck (1826-1855), the first Black to graduate from an American medical school

Between 1844 and 1846, David Peck studied medicine under Dr. Joseph P. Gaszzam, a white anti-slavery doctor in Pittsburgh. He then entered Rush Medical College in Chicago in 1846, three short years after the institution opened. Upon graduation in 1847, Peck became the first Black man to graduate from an American medical school.
In 1849, Peck established his practice in Philadelphia. Peck’s medical practice, however, was not successful. Few doctors recognized his status, referred patients to him or consulted with him. He returned to Pittsburgh in 1850. Peck was notable in having toured Ohio with William Lloyd Garrison and Frederick Douglass, promoting abolitionist ideals. Peck moved to Nicaragua in early 1852 where he was killed in 1855.
Dr. Daniel Hale Williams (1858-1931), physician, pioneer of heart surgery and founder of National Medical Association

Daniel Hale Williams was born in Hollidaysburg, PA, and he earned his M.D. from Northwestern University in 1883. He organized the Provident Hospital and Training School for Nurses in 1891, the first black-owned hospital in the United States.
In 1893, Williams performed the first successful closure of a wound of the heart and pericardium (the layer immediately surrounding the heart). President Cleveland appointed him surgeon in chief of Freedmen’s Hospital, Washington, D.C. During his five-year tenure there, he reorganized the hospital and established a training school for African-American nurses.
Williams helped form the National Medical Association in 1895, though African-Americans were denied membership at that time. He was a charter member of the American College of Surgeons, being the first and only Black member for many years. From 1899 until his death, he was professor of clinical surgery at Meharry Medical College, Nashville, TN.
Mary Eliza Mahoney (1845-1926), groundbreaking nurse

America’s first Black professionally trained nurse, Mary Eliza Mahoney, was born in Dorchester, Massachusetts. She graduated from the New England Hospital for Women and Children Training School for Nurses in 1879, having worked there for 15 years before being accepted into its nursing school.
After gaining her nursing diploma in 1905, Mahoney worked for many years as a private care nurse, serving as director of the Howard Orphan Asylum for Black children in Kings Park, Long Island, NY. In 1896, Mahoney was one of the original members of a predominantly white Nurses Associated Alumnae of the United States and Canada, which became the American Nurses Association (ANA) in 1911. In 1908, she was cofounder of the National Association of Colored Graduate Nurses (NACGN).
Dr. Charles R. Drew (1904-1950), physician, pioneer of blood transfusions

Charles Richard Drew was born in Washington, D.C. As a surgeon and a professor at Howard University, he developed a means of preserving blood plasma for transfusion. During World War II he headed the program that sent blood to Great Britain. Among his noteworthy accomplishments, Drew started and was the first Director of the American Red Cross Blood Bank.
Dr. Louis Sullivan (1933- ), Physician and 17th Secretary of the U.S. Department of Health and Human Services

Louis W. Sullivan was born in Atlanta, Georgia. Sullivan earned his medical degree, cum laude, from Boston University in 1958. Dr. Sullivan held positions at Harvard Medical School and other facilities. In 1967, he founded the Boston University Hematology Service at Boston City Hospital and later was director of the Boston Sickle Cell Center.
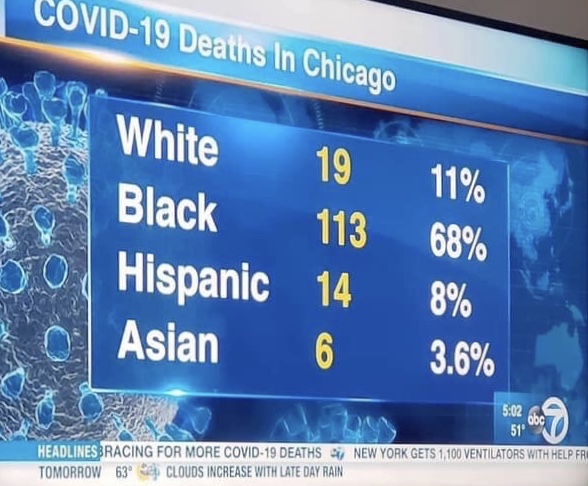
Dr. Sullivan left Boston in 1975 to become the founding dean and director of the Medical Education Program at Morehouse College. In 1985, the Morehouse School of Medicine was fully accredited as a four-year medical school. In 1989, Dr. Sullivan took a leave of absence from Morehouse to become the 17th Secretary of Health and Human Services. As Secretary, Dr. Sullivan championed causes among vulnerable populations. He was a strong advocate for increased medical research pertaining to racial and ethnic minorities and the illumination of racial healthcare disparities.
Dr. Ben Carson (1951- ), Groundbreaking neurosurgeon

Dr. Carson is a contemporary addition to this list because of his achievements, including successfully detaching twins conjoined at the head in 1987 and his groundbreaking surgery on a twin suffering from an abnormal expansion of the head — conducted while the baby was still in the mother’s uterus. Dr. Carson has performed operations which have greatly expanded scientific knowledge of the brain and its functions. Dr. Carson was the youngest and long-time director of pediatric neurosurgery at Johns Hopkins Hospital in Baltimore. His clinical expertise in treating rare neurological conditions is unquestioned and largely unparalleled.
Congratulations to these and the many other who are pioneers and leaders. Let’s support and encourage the many who continue this proud tradition.
Feel free to ask your SMA expert consultant any questions you may have on this topic.
Order your copy of Dr. Sterling’s new book Behind The Curtain: A Peek at Life from within the ER at jeffreysterlingbooks.com, iTunes, Amazon, Barnes and Nobles and wherever books are sold.
Thanks for liking and following Straight, No Chaser! This public service provides a sample of what http://www.SterlingMedicalAdvice.com (SMA) and 844-SMA-TALK offers. Please share our page with your friends on WordPress, like us on Facebook @ SterlingMedicalAdvice.com and follow us on Twitter at @asksterlingmd.
Copyright © 2017 · Sterling Initiatives, LLC · Powered by WordPress