Dehydration is one of those topics that illustrates the adage “a little knowledge is a dangerous thing”— except I would adjust that to suggest a little of the wrong type of knowledge is dangerous. In this Straight, No Chaser, we’ll provide you with enough information to recognize and act on dehydration when it becomes significant or severe, because the first thing you should know is dehydration can be a life-threatening emergency. In fact dehydration due to diarrheal diseases remains the one of the topic five causes of death in the world.
Simply put, you’re dehydrated when your body is lacking in the amount of fluids it needs. This can occur from losing fluid (as occurs with excessive vomiting, diarrhea, sweating, urination or other losses), from insufficient fluid intake (as occurs with nausea, a loss of appetite, eating disorders, etc.) or from a combination of both.
Let’s approach the rest of the conversation simply by answering seven commonly asked questions.
1. Who’s at risk/what places me at risk?

Infants, children, the elderly and the ill are at particular risk for dehydration (and add yourself if you work outdoors during hot summer months). Children simply have lower fluid amounts than adults, and fluid losses is kids proportionately cause greater effects. All the above risk groups share the habit of a more rapid utilization and/or turnover of fluids, requiring higher fluid intake.
2. How can I prevent dehydration?
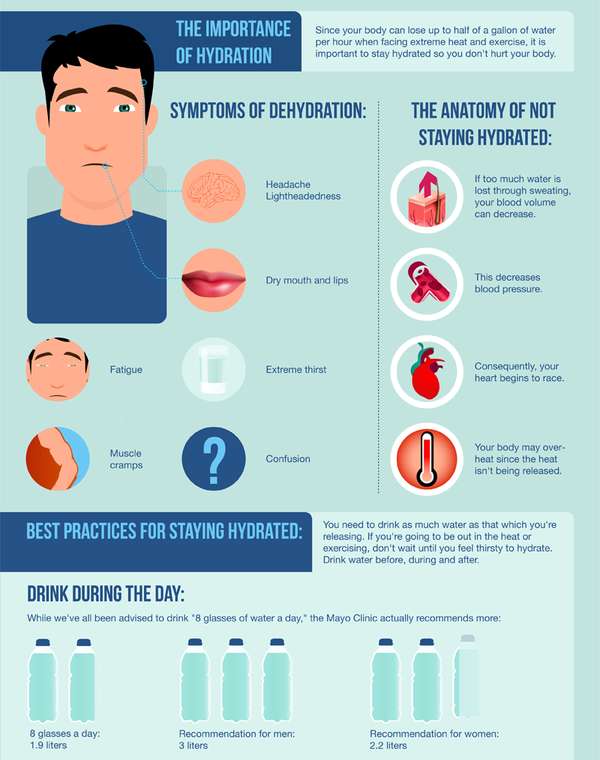
This is relatively easy. Drink plenty of fluids every day and even more when exercising or losing fluids (e.g., menstruating, sweating on hot days, exercising or if you’re suffering from vomiting or diarrhea).
3. How can I recognize when I’m dehydrated?
You will do a good job of preventing dehydration if you learn the early signs, including those less severe items listed in the above picture. You will do an even better job if you don’t wait until signs develop to begin rehydration. Specifically, sipping fluids is generally recommended for anyone with vomiting, diarrhea or a febrile illness.
4. When should I treat possible dehydration?
Here are a few scenarios that should prompt treatment.
- There is less frequent wetting of diapers in children and urination in those older.
- There is a relative absence/reduction of saliva and/or tears.
- In infants, the eyes or the soft spot on the top of the head (the fontanelles) may be sunken.
- You’re having diarrhea and/or vomiting, particularly when you seemingly can’t keep any food down.
5. How can I treat my dehydration?
Here are some key points for you to understand.
- IV fluids may be necessary for moderate to severe dehydration. However, IV fluids are not necessary to treat most cases of dehydration. In fact, IVs are rarely used to treat dehydration in the rest of the world outside of the U.S.
- You will do much better treating dehydration if you sip instead of guzzle. If you’re vomiting, and your stomach is “upset,” you likely will precipitate more vomiting if you take in large amounts of fluids at a time. Think in terms of teaspoons or syringes of fluid.
- You may have heard that electrolyte solutions aren’t the best for rehydrating yourself, but in fact water replacement without electrolytes isn’t what you want to attempt ideally. All things considered, electrolyte solutions and “freezer pops” are very effective for basic considerations of addressing hydration.
- The next time you’re at your local pharmacy, ask the pharmacist to show you some rehydration solutions. These are especially effective.
6. When do I need to see a physician for dehydration?
You or your loved one may be in the midst of a life-threatening condition if you’re light-headed, confused, dizzy, lethargic or have blacked out. This should prompt a 911 call or an immediate visit to the emergency room.
There are multiple other symptoms that should prompt you to contact your physician. Here are some of them, in addition to those listed in the previous questions.
- You are sick and can’t keep down fluids, even when you’re sipping.
- Vomiting has continued for more than 24 hours in an adult or more than 12 hours in a child.
- Diarrhea has continued for more than five days.
- You have bloody stools or vomit.
- You notice an abnormally fast heartbeat.
- Your infant has dry skin that sags back into position slowly when pinched up into a fold.
- You or your child has little or no urine output for eight hours.
- You notice irritability or less activity in your infant or child.
7. What’s the worst that can happen?
Dehydration can lead to death and other severe disturbances, including coma, brain damage, seizures, and shock. Just understand that if you think you could be dehydrated, you should be drinking fluids.
Remember: dehydration is something seemingly simple that can go horrible wrong if unattended. The better news is when you do enact preventive and early treatment measures, outcomes are generally very good. Feel free to refer to this information when the need arises. You can always contact your SMA expert consultant at www.sterlingmedicaladvice.com or 844-SMA-TALK for any questions you have on this or any other topic.
Feel free to ask your SMA expert consultant any questions you may have on this topic.
Order your copy of Dr. Sterling’s new book Behind The Curtain: A Peek at Life from within the ER at jeffreysterlingbooks.com, iTunes, Amazon, Barnes and Nobles and wherever books are sold.
Thanks for liking and following Straight, No Chaser! This public service provides a sample of what http://www.SterlingMedicalAdvice.com (SMA) and 844-SMA-TALK offers. Please share our page with your friends on WordPress, like us on Facebook @ SterlingMedicalAdvice.com and follow us on Twitter at @asksterlingmd.
Copyright © 2016 · Sterling Initiatives, LLC · Powered by WordPress