Let’s put this take home message up front: here’s a pretty good demonstration of the value of vaccines. I hope that each of you resolves to get any children you care for vaccinated before they become sexually active.
I want to thank my friend and colleague, Dr. Julius Ellis, noted Ob/Gyn physician for contributing to this post. Let’s start this with two simple statements:
- Cervical cancer has basically been shown to be caused by an infection.
- There soon will be no reason that anyone has to have cervical cancer.
As a reminder, the cervix is the lower and narrow end of the uterus that connects the vagina to the upper part of the uterus (i.e. the womb). Cervical cancer used to be the leading cause of cancer death for women in the US.
In 2011 (the most recent year numbers are available):
- 12,109 women in the United States were diagnosed with cervical cancer.
- 4,092 women in the United States died from cervical cancer.
Fortunately, over the last 40 years, the number of cases of cervical cancer and the number of deaths from cervical cancer have decreased significantly, largely due to Pap tests. The even better news is the opportunity exists to virtually eradicate the disease. Cervical cancer is highly preventable because screening tests and a vaccine to prevent human papillomavirus (HPV) infections are available. When cervical cancer is found early, it is highly treatable and associated with long survival and good quality of life.
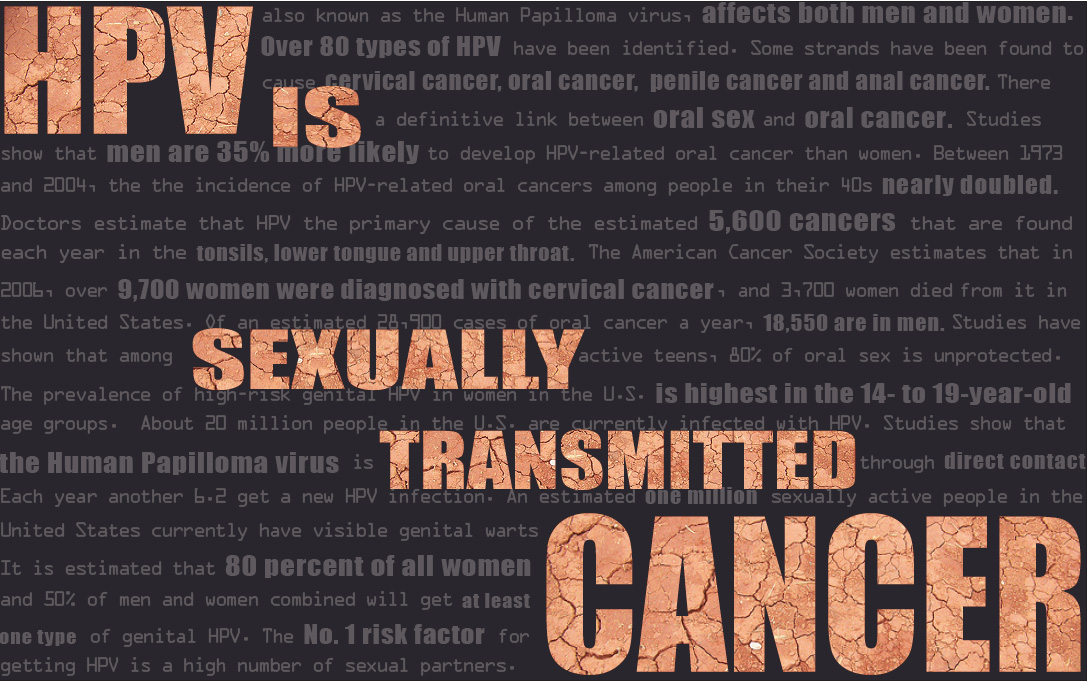
Yes, cervical cancer is a sexually transmitted infection (STI), and the most common STI is now known to be caused by the human papillomavirus (HPV). Some of you will recognize HPV as a cause of genital warts. This means if you ever develop warts, go get checked immediately (another good reason to do this is because genital syphilis may also present as warts). Even more importantly, certain HPV strains have been shown to cause virtually all cervical and anal cancers. HPV also causes some cancers of the vagina, penis, and oropharynx (a certain part of the throat—and yes, this is what Michael Douglas was referencing about having obtained throat cancer by performing oral sex).
Early on, cervical cancer may not cause signs and symptoms, but advanced cervical cancer may cause bleeding or discharge from the vagina, either of which may be persistent or abnormal from similar episodes you’ve had in the past. If you have any of these signs, see your physician for an evaluation of this and other possible causes of these symptoms.
Am I at risk for HPV? How do you get this?
Everyone having sex or who has ever had sex is at risk for HPV. In fact, nearly all sexually active men and women get it at some point in their lives. HPV is passed on through genital contact, most often during vaginal and anal sex, but also through oral sex and genital-to-genital contact without intercourse. HPV can be passed on between straight and same-sex partners even if and when the infected person has no signs or symptoms. It’s important to know there’s a big difference between obtaining the HPV virus and obtaining cancer from having the HPV virus.
If I get genital warts, will I get cancer?
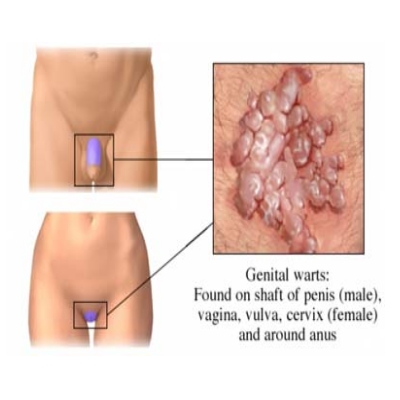
Not necessarily, but the possibility is high enough that you need to get treated. Most HPV infections actually resolve on their own. It’s the ones that linger that pose particular concern.
If I do have warts, what increases my risks for these cancers?
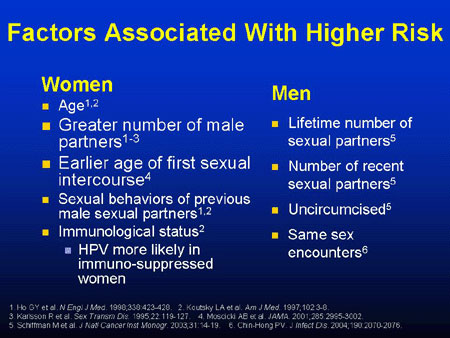
Smoking, a weakened immune system, having had many children (for increased risk of cervical cancer), long-term oral contraceptive use (for increased risk of cervical cancer), and poor oral hygiene (for increased risk of oropharyngeal cancer) all increase the risk for developing cancer after a HPV infection.
How do I get this and how do I prevent it?
The most reliable way to prevent infection with HPV is abstinence, avoiding any skin-to-skin oral, anal, or genital contact with another. If you are sexually active, a long-term, mutually monogamous relationship with an uninfected partner is the strategy most likely to prevent HPV infection. However, because of the lack of symptoms, it’s hard to know whether a partner is currently infected with HPV. Use of condoms reduces the transmission of HPV between partners, although areas not covered by a condom can still be infected.
The Food and Drug Administration (FDA) has approved two HPV vaccines, branded as Gardasil (for the prevention of cervical, anal, vulvar, and vaginal cancer, precancerous lesions, and genital warts in these areas) and Cervarix (for the prevention of cervical cancer and precancerous cervical lesions caused by HPV). Both vaccines are highly effective, but neither has been approved for prevention of penile or oropharyngeal cancer. And yes, it’s safe and effective as young as age 9, although the Center for Disease Control and Prevention currently recommends vaccination between ages 11–14. You must contact your physician for additional details on these important medications.
How do I treat HPV infections?
There’s no treatment for HPV itself, but the problems HPV causes can be treated. We’ll address the two major ones:
- Genital warts may be treated topically by you or a healthcare provider. If not treated, they may multiply, go away, or stay the same.
- Cervical cancer may be treated by your gynecologist, but be warned: Prevention is best, and early detection gives you the best chance for the best outcomes. Continue those annual exams.
There will soon come a time when all boys and girls are receiving vaccinations at around ages 11–12, and cervical cancer (in particular) will become a rare entity. That only happens if you get your family immunized. The science is in. There’s no good reasons left to wait.
Thanks for liking and following Straight, No Chaser! This public service provides a sample of what 844-SMA-TALK and http://www.SterlingMedicalAdvice.com (SMA) offer. Please share our page with your friends on WordPress, Facebook @ SterlingMedicalAdvice.com and Twitter at @asksterlingmd.
Copyright © 2014 · Sterling Initiatives, LLC · Powered by WordPress.