Here’s a pretty common scenario. You’re a first time parent with the most adorable kid in the world. You’re in full tiger mom or dad mode, and you’re not going to let anything in the world hurt your baby. Your child has a sore throat, and you’re worried that it could be strep throat. You want to know if s/he needs antibiotics (Actually, you’re demanding antibiotics, but that’s another conversation!).
If a physician is actually using evidence based medicine to treat you instead of just throwing antibiotics at you to make you feel better (We call that ‘treating the parents’), there are criteria (based on what is called a Centor score) that determines when antibiotics are indicated and will make a difference (because most sore throats are caused by viruses and don’t respond to antibiotics; they’ll get better on their own in time). The Centor score is simple enough that you could figure it out yourself. Here are the components.
The patients are judged on six criteria, with one point added for each positive component.
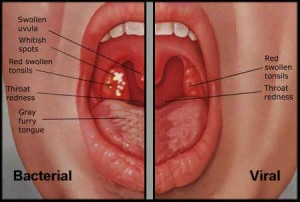
- History of fever
- Tonsillar exudates (those white patches in the back of the throat)
- Tender anterior cervical lymph nodes (those swollen lumps in the upper neck right below the angle of the jaw)
- No coughing
- Age <15 add 1 point (because strep is more likely at this age)
- Age >44 subtract 1 point (because strep is way less likely at this age)
After that, you’ll have a number. Physicians use that number to guide management as follows:
- 0 or 1 points – No antibiotic or throat culture is necessary; the risk of strep. infection is less than 10%.
- 2 or 3 points – A throat culture should be done, and the patient should be treated with an antibiotic if the culture is positive.
- 4 or 5 points – The patient should be treated with an antibiotic (The risk of strep. infection is 56%), and no throat culture needs to be done.
So… if you do this calculation at home and get a 0 or 1, don’t expect antibiotics, and don’t get mad when you don’t get them. There are consequences to inappropriate usage of antibiotics. As I’ve discussed in the past (as with Staph becoming MRSA, for example), antibiotic resistance is a real phenomenon with dangerous ramifications for patients. At a patient, you really don’t want to take medications unnecessarily. Microorganisms develop resistance when you’re taking medications inappropriately. You want to remain such that when you need them, they work.
I’m happy to answer any questions or take any comments. Thank you.
Copyright © 2013 · Sterling Initiatives, LLC · Powered by WordPress