Introduction

This Straight, No Chaser post reviews a few common skin rashes. The guide features in-depth discussion on several of them.
Common Skin Rashes
Here are a few of the more common skin rashes. There are many additional rashes and conditions not covered in this brief guide. This include patterns seen in sexually transmitted infections. If you have any questions or concerns about your condition, please consult a physician. Click the links for additional posts discussing them in detail.
Contact dermatitis

Have you ever been affected by poison ivy, poison oak or sumac? Has costume jewelry (most likely containing nickel) made you break out? Contact with chemicals to which the patient is allergic or with skin irritants cause this condition. Contact dermatitis can occur anywhere there’s contact with an irritant or allergen. It tends to be weepy and oozy. Furthermore, it may discolor this skin.
Diaper rash
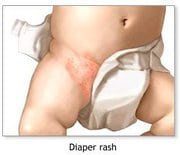
Diaper rash is an irritant contact dermatitis caused by prolonged exposure to urine and/or feces. The rash occurs due to entrapment by a diaper or other restrictive garments. You’ll see it in the distribution of the diaper.
Drug eruptions

Drug eruptions represent a wide range of rashes brought on by antibiotics and other medicines. The lesions are mostly non-specific and will resolve with stopping use of the medicine.
Eczema (Atopic dermatitis)

The lesions of eczema are red itchy, weeping rashes. They are most commonly seen on the inner aspects of the elbows and in back of the knees. They also are seen on the cheeks, neck, wrists, and ankles. Eczema is commonly found in patients who also have asthma and/or hay fever.
Hives (urticaria)

Hives are red bumps and wheals that commonly are causes by drug exposure. They appear and resolve suddenly, most typically in about eight hours. Due to the risk of recurrence and breathing difficulty, drugs and foods that cause these should be avoided once identified.
Miliaria (heat rash)

Heat rash is caused by blocked sweat ducts, which occurs most commonly during hot and humid temperatures. These rashes resemble small blisters or acne-like lesions. Also, heat rash is more likely to occur in areas that can’t release heat as easily. These areas include the groin, elbow creases, under breasts and around the neck and upper chest. Getting to a cooler environment is often sufficient treatment.
Psoriasis

Psoriasis is recognizable due to silvery flakes of skin, most commonly occurring on the elbows, knees and scalp.
Seborrheic dermatitis

Seborrhea is the most common adult rash. You’ll see a scaly, itchy and red rash that is most likely located on the scalp, forehead, eyebrows, cheeks, and ears. In infants, it may involve the scalp and diaper area.
Stasis dermatitis

Stasis dermatitis is often seen in individuals with poor circulation in the veins. It’s a weepy, oozy rash that occurs on the lower legs of those affected.
General Treatment Considerations
In the absence of other symptoms, it is perfectly reasonable to wait a few days to see if most rashes resolve on their own. Also, it’s reasonable to treat symptoms such as itching and dry skin with over-the-counter remedies.
Consider the following:
- Anti-itch creams containing 1% hydrocortisone cream can be helpful.
- Oral antihistamines, including diphenhydramine (eg. Benadryl) and hydroxyzine can be helpful for itching. However, you should be careful about side effects, including drowsiness, which can affect your function and operation of machinery.
- Moisturizing lotions are always a good choice. They prevent the dryness and cracking of skin that can lead to infections.
- Antifungal medications are useful for athlete’s foot, jock itch or other obvious common fungal infections. These medicines tend to contain clotrimazole (Lotrimin), miconazole (Micatin), or terbinafine (Lamisil).
If these measures aren’t successful, if the rash persists, or if it becomes more widespread, you should consider visiting a physician or dermatologist.
Follow us!
Ask your SMA expert consultant any questions you may have on this topic. Also, take the #72HoursChallenge, and join the community. Additionally, as a thank you, we’re offering you a complimentary 30-day membership at www.72hourslife.com. Just use the code #NoChaser, and yes, it’s ok if you share!
Order your copy of Dr. Sterling’s books There are 72 Hours in a Day: Using Efficiency to Better Enjoy Every Part of Your Life and The 72 Hours in a Day Workbook: The Journey to The 72 Hours Life in 72 Days at Amazon or at www.jeffreysterlingbooks.com. Another free benefit to our readers is introductory pricing with multiple orders and bundles!
Thanks for liking and following Straight, No Chaser! This public service provides a sample of http://www.SterlingMedicalAdvice.com (SMA) and 844-SMA-TALK. Likewise, please share our page with your friends on WordPress! Also like us on Facebook @ SterlingMedicalAdvice.com! Follow us on Twitter at @asksterlingmd.
Copyright ©2013- 2019 · Sterling Initiatives, LLC · Powered by WordPress






